
However, collecting 24-h urine samples for hydration assessment in real-life is methodologically difficult and burdensome, especially in children. Moreover, urine osmolality provides an indication of arginine vasopressin (AVP) levels, the main regulator of water homeostasis. A 24-h urine sample is recommended to assess daily hydration with urinary biomarkers as it is valid, noninvasive method, and represents the behavioral and neuroendocrine responses throughout an entire day. Hydration can be assessed by using different blood (plasma osmolality, plasma copeptin, plasma sodium, urea nitrogen/creatinine ratio) and urine (urine osmolality, urine specific gravity, urine color, urine volume, void frequency) biomarkers, body mass changes, or thirst, considering body weight loss as gold standard marker during exercise. Thus, it is important for health care practitioners to incorporate hydration assessment into practice when evaluating overall children’s’ health. Interestingly, a large proportion of children in the United States exhibit elevated urine concentration (assessed via urine osmolality) suggesting that they might be underhydrated. For instance, children with normal body weight seem to have better hydration compared with obese, while increasing water intake improves cognitive performance. Adequate hydration or drinking water is reported to be associated with children’s health benefits. Children may be more susceptible to the adverse effects of underhydration and may be at greater risk. Low water intake and underhydration are associated with various health issues such as increased risk of kidney disease, diabetes, obesity, and impaired cognitive function.

Water is a solvent for protein synthesis, and it helps the hydrolytic reactions for macronutrients, waste elimination, and thermoregulation. This data will have practical implication for health care professionals and researchers.Ībout 55–70% of the human body consists of water, which plays a vital role as a structural component of cells, tissues, and organs. These data suggest that in free-living healthy children, 24-h urine concentration may be approximated from a late afternoon spot urine sample.
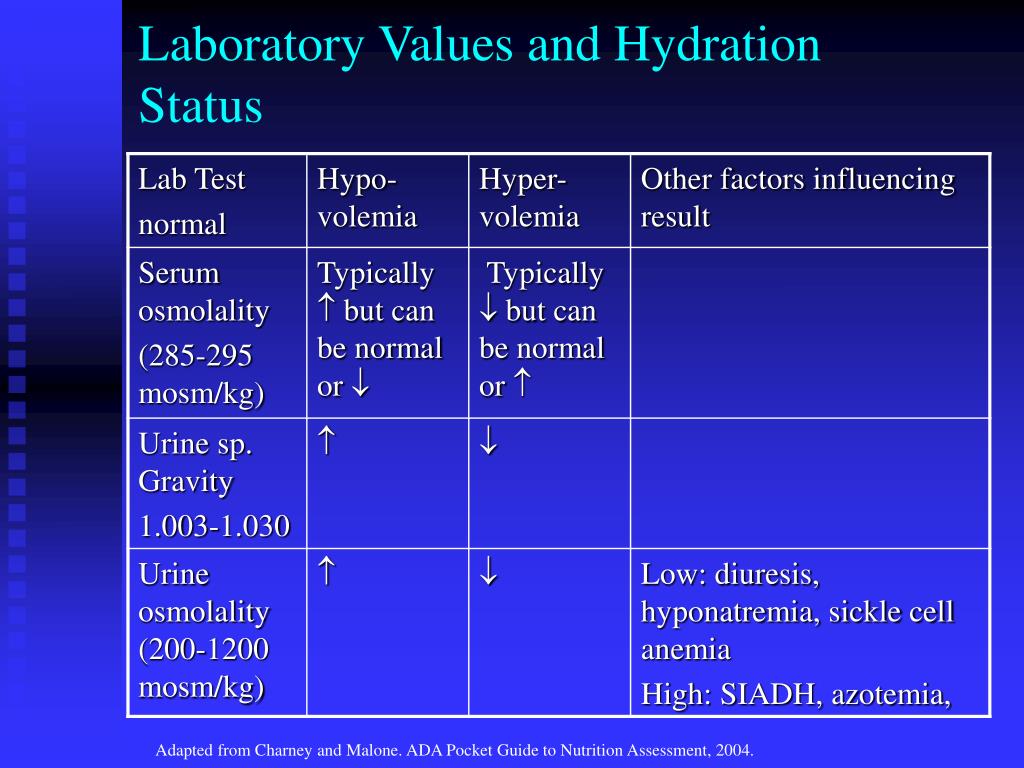
The overall diagnostic ability of urine osmolality assessed at late afternoon (1600–1959) to diagnose elevated urine osmolality on the 24-h sample was good for both cutoffs of 800 mmol kg −1 and 500 mmol kg −1 (AUC: 83.5% sensitivity: 75.0% specificity: 80.0% threshold: 633 mmol kg −1). Late afternoon (1600–1959) spot urine sample UOsm value was equivalent to the 24-h UOsm value in children ( P < 0.05 mean difference: 62 mmol kg −1 95% CI: 45–78 mmol kg −1). Subjects/MethodsĪmong 541 healthy children (age: 3–13 years, female: 45%, 77% non-Hispanic white, BMI:17.7 ± 4.0 kg m −2), UOsm at specific time-windows was compared with UOsm from the corresponding pooled 24-h urine sample using an equivalence test. The aim of the present study was to examine whether urine osmolality (UOsm) assessed from a spot urine sample in specific time-windows was equivalent to 24-h UOsm in free-living healthy children. It has been demonstrated that afternoon spot urine samples are most likely to provide equivalent urine concentration to 24-h urine samples in adults. However, urine output is subject to circadian variation, with urine being more concentrated in the morning. While daily hydration is best assessed in 24-h urine sample, spot sample is often used by health care professionals and researchers due to its practicality.


 0 kommentar(er)
0 kommentar(er)
